Introduction
This brief examines the complex ecosystem of collaborators involved in implementing Food Is Medicine (FIM) programs through health-related social needs (HRSN) policies in Medicaid. It analyzes the roles and interactions of state Medicaid agencies, Medicaid managed care organizations (MCOs), health care providers, and community-based organizations (CBOs) in four states implementing FIM initiatives: California, Michigan, New York, and North Carolina.
Drawing on state policy, it identifies effective practices and key challenges in FIM implementation, exploring how different partners collaborate to integrate food-based interventions into their Medicaid programs. Furthermore, the brief situates current FIM initiatives within the broader context of the evolving HRSN field. By synthesizing recent research and on-the-ground experiences, it highlights areas for further study, policy development, and program considerations.
Terms and Definitions
Community-Based Organization (CBO)
A local entity that is typically nonprofit and focuses on addressing various social, economic, health, and educational issues within their specific locality
Food Is Medicine (FIM)
Encompasses a broad range of approaches that promote optimal health and healing and reduce disease burden by providing nutritious food – in conjunction with human services, education, and policy change – through collaboration at the nexus of health care and community.
Health-related Social Needs (HRSN)
Social and economic needs that individuals experience that affect their ability to maintain their health and wellbeing. These include needs such as employment, affordable and stable housing, healthy food, personal safety, transportation, and affordable utilities.
Medicaid Managed Care Organization (MCO)
Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations (MCOs) that accept a set per member per month (capitation) payment for these services.
Key Collaborators
FIM initiatives have gained significant traction in recent years, with a growing number of government agencies, health care providers, and philanthropic organizations embracing the concept of using nutrition-based interventions to prevent and manage chronic health conditions.
At the federal level, the U.S. Department of Health & Human Services (HHS) and the Centers for Medicare & Medicaid Services (CMS) have taken steps to allow state Medicaid programs to offer Food Is Medicine services. Ten states have already received approval from CMS to implement Section 1115 Demonstrations that allow them to implement food-based interventions for certain Medicaid beneficiaries, ranging from medically tailored meals to produce prescription programs.
Beyond Medicaid, the U.S. Department of Agriculture provides grant funding for produce prescription programs through the Gus Schumacher Nutrition Incentive Program (GusNIP). Additionally, the Department of Veterans Affairs (VA) has partnered with the Rockefeller Foundation to launch a similar initiative aimed at improving the health and well-being of Veterans by providing them with access to fresh produce and nutrition education. As policymakers and health care leaders continue to explore ways to integrate food-based interventions, the coming years are likely to bring even greater expansion and innovation in the Food Is Medicine space.
The implementation of Food Is Medicine programs involves a complex network of collaborators across various levels of government, the health care sector, and the community. The following section presents case studies examining the roles of state Medicaid agencies; managed care organizations (MCOs); health care providers; and community-based organizations (CBOs) in North Carolina, California, New York, and Michigan.
These states have each adopted distinct approaches to integrating food-based interventions into their Medicaid programs. By analyzing the strategies and partnerships in these distinct health-related social needs interventions, the following sections explain the intricate ecosystems implementing Food Is Medicine programs.
Case Studies
Case Study 1: North Carolina
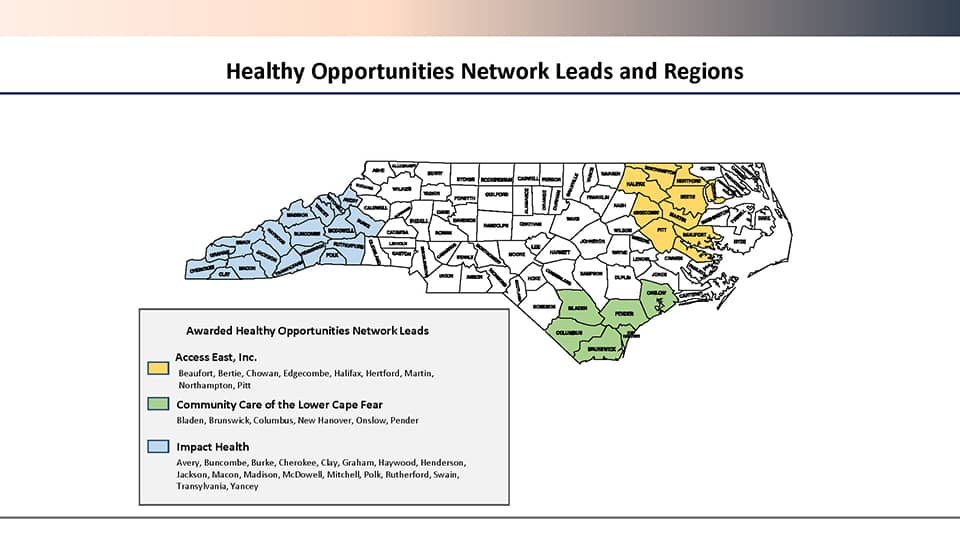
North Carolina’s Healthy Opportunities Pilots (HOP) program was among the first in the country to address health-related social HRSNs through a Section 1115 Demonstration Waiver. Overseen by the North Carolina Department of Health and Human Services (NC-DHHS), Healthy Opportunities Pilot operates in 3 pilot regions illustrated in the graphic below, each managed by a designated Network Lead:
- Impact Health in Western NC
- Access East in Eastern NC
- Community Care of the Lower Cape Fear in the Cape Fear Region
Before launching Pilot services, the state Medicaid agency procured 3 Network Leads (1 per Pilot region) with deep roots in their communities to facilitate collaboration and build partnerships across health care payers and human service providers.
At the heart of the program are Human Service Organizations (HSOs), community-based organizations contracted by Network Leads to provide a range of social services and food-related services, such as Supplemental Nutrition Assistance Program (SNAP) enrollment assistance, group nutrition classes, produce prescriptions, healthy food boxes, and medically tailored meals.
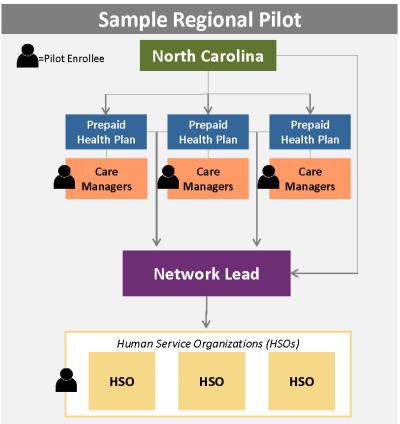
Eligible individuals must be North Carolina Medicaid Managed Care members, living in a Pilot region county, with at least 1 qualifying physical or behavioral health condition and 1 qualifying social risk factor, such as food insecurity. Care managers (based at a Prepaid Health Plan [PHP] or Designated Care Management Entity), play a crucial role in program implementation by interfacing with Medicaid members and PHPs to conduct care management, assess member eligibility for services, and track member progress.
Highlight of Collaborator Roles in North Carolina
NC Department of Health and Human Services
- Programmatic oversight
- Contract with Prepaid Health Plan
Prepaid Health Plans
- Approve member eligibility for services
- Authorize services
- Provide funding for services delivered
Care Managers
- Conduct care management
- Assess member eligibility for services
- Track member progress
Network Leads
- Contract with NC-DHHS and Prepaid Health Plan to develop and manage a network of Human Service Organizations
Human Services Organizations
- Contracted by Network Leads to deliver services
This flow chart shows the relationships between HOP pilot entities.
Moving Forward
Leveraging existing HOPs infrastructure and experience, NC-DHHS seeks to renew all previous components of the program while expanding access to services that address HRSNs for residents across the state. A noteworthy modification in the renewal proposal is the request to allow PHPs and Human Service Organizations to contract directly with each other under specific conditions, provided that both parties have demonstrated readiness and willingness to engage in such arrangements.
For some Human Service Organizations, this refinement would remove the Network Lead as an intermediary between Prepaid Health Plans and Human Services Organizations, enabling direct collaboration between the 2 entities for service provision.
Case Study 2: California
The California Advancing and Innovating Medi-Cal (CalAIM) initiative, spearheaded by the California Department of Health Care Services (DHCS), represents a groundbreaking effort to integrate food and nutrition services into Medi-Cal, the state's Medicaid program.
A key feature of this initiative is Community Supports (CS) [PDF - 544 KB], medically appropriate, cost-effective alternatives that Medi-Cal Managed Care Plans (MCPs) can opt to provide in lieu of services (ILOS) covered under Medi-Cal. Managed Care Plans administer Community Supports [PDF - 895 KB], contracting [PDF - 312 KB] local providers or organizations with experience in delivering Community Supports services and an existing footprint in the communities they serve. Their role in identifying eligible enrollees, overseeing service provision, and managing reimbursements [PDF - 670 KB] is critical for the sustainable implementation of Community Supports within the Medi-Cal system.
At the forefront of service delivery are Community Supports providers, leveraging community connections to reach underserved populations effectively. Community Supports providers with a state-level Medi-Cal enrollment pathway are required to enroll as a Medi-Cal provider [PDF - 359 KB]; those without such a pathway must undergo vetting by the Managed Care Plans to participate.
Highlight of Collaborator Roles in California
Department of Health Care Services (DHCS)
- Programmatic oversight
Managed Care Plans (MCPs)
- Contracted by Department of Health Care Services (DHCS) to administer Community Supports
- Identify and refer eligible members
- Contract with and oversee Community Supports providers
- Ensure information technology infrastructure and data analytic capabilities
- Submit encounter data to Department of Health Care Services
Community Supports (CS) Providers
- Contracted by Managed Care Plans (MCPs) to provide Community Support services
- Submit claims to Managed Care Plans for transmissions to Department of Health Care Services (DHCS); if not able, submit invoices to Managed Care Plans
Case Study 3: New York
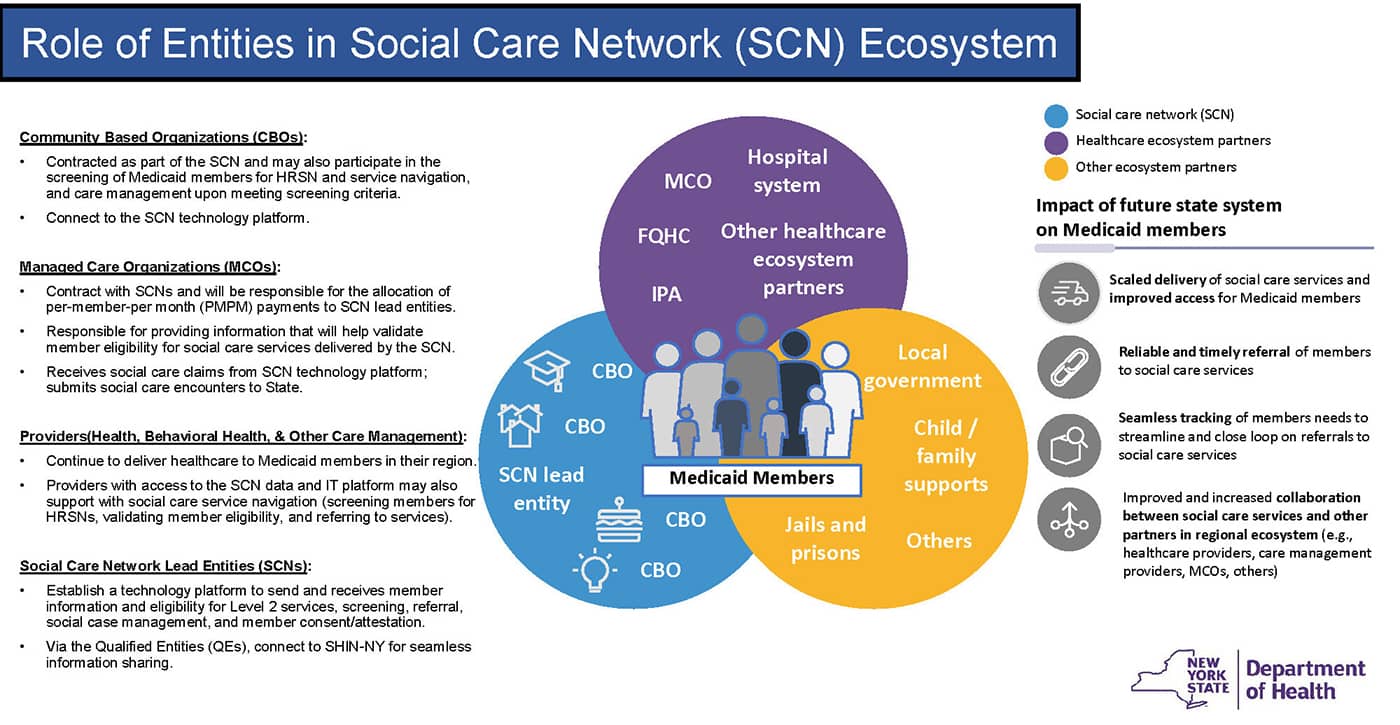
The New York State Department of Health (NYS DOH) recently approved New York Health Equity Reform (NYHER) 1115 Medicaid Waiver, a transformative initiative aimed at addressing health disparities and advancing health equity across the state. Recognizing the expansive and diverse nature of New York, the waiver divides the state into 9 regions, aligning with established Medicaid rate-setting territories.
At the heart of this reform are Social Care Networks (SCNs), which will be contracted by managed care organizations in each region to create and oversee networks of community-based organizations to provide approved health-related social needs services. To facilitate data exchange and enhance care coordination, SCNs will integrate with the Statewide Health Information Network for New York (SHIN-NY), a social care information technology platform.
The waiver also introduces Health Equity Regional Organizations (HEROs), independent statewide entities tasked with developing regionally focused approaches to reduce health disparities through data aggregation, regional needs assessments, collaborator engagement, support for value-based payment models, and program evaluation.
Highlight of Collaborator Roles in New York
New York State Department of Health
- Programmatic oversight
- Per member per month (PMPM) payments to managed care organizations (MCOs)
- Infrastructure funds to Social Care Networks (SCN)
Health Equity Regional Organizations (HEROs)
- Contracted by New York State Department of Health
- Data aggregation
- Regional needs planning
- Collaborator engagement
- Value-based payment recommendations
- Program evaluation
Managed Care Organizations (MCOs)
- Contract with Social Care Networks (SCNs) for health-related social need services and pay per member per month rates
- Provide data to validate member eligibility for health-related social need services
Social Care Networks
- Contracted by managed care organizations to establish and manage a network of community-based organizations
- Contract with Statewide Health Information Network for New York (SHIN-NY) for referral management
- Contract with community-based organizations for health-related social need services and pay fee-for-service
Community-Based Organizations (CBOs)
- Contracted by Social Care Networks (SCNs) to provide services, screening, navigation, and care management
Case Study 4: Michigan
The Michigan Department of Health and Human Services (MDHHS) will provide Medicaid Health Plans (MHPs) with the opportunity to offer ILOS [PDF - 193 KB] that address members’ food and nutrition-related needs. This program aims to enhance the state’s current food and nutrition initiatives, with the goal of improving health outcomes and decreasing the need for future medical care by tackling food insecurity and facilitating access to healthy food options.
Participation is limited to Medicaid Health Plans that are part of Michigan’s Comprehensive Health Care Program (CHCP), the state’s Medicaid managed care initiative that operates alongside the Healthy Michigan plan, the state’s Medicaid expansion program.
Medicaid Health Plans will contract with community-based organizations that possess the necessary experience and expertise to deliver ILOSs, ensuring that at least 30 percent of services are provided by community-based organizations that have one or more locations in Michigan and are engaged in the state's food economy. ILOS providers will be required to enroll in Michigan’s Community Health Automated Medicaid Processing System (CHAMPS) for program participation and reimbursement.
As of July 2024, Michigan is actively engaged in the planning and development phase for the implementation of ILOS. Michigan Department of Health and Human Services (MDHHS) received responses from numerous external partner organizations to its Request for Information (RFI) [PDF - 320 KB] released in March 2024, which indicated overall support for the proposed nutrition-focused services and potentially eligible populations.
Additionally, the MDHHS published an online structured survey [PDF - 2.4 MB] soliciting input on the In Lieu of Services (ILOS) Policy Guide Draft [PDF - 607 KB] by the end of July 2024, outlining the operational requirements and recommendations to assist Medicaid Health Plans and ILOS providers in effectively administering and delivering these services.
Highlight of Collaborator Roles in Michigan
Michigan Department of Health and Human Services (MDHHS)
- Programmatic oversight
MHPs
- In Lieu of Services (ILOS) implementation
- Eligibility, referral, and authorization
- Contract with In Lieu of Services providers or contract with an entity to develop and maintain In Lieu of Services provider network
In Lieu of Services Providers
- Service provision
Implementation Perspectives
Existing policy on the implementation of Food Is Medicine initiatives underscores the vital roles played by various collaborators, including state Medicaid agencies, managed care organizations, health care providers, and community-based organizations. Each of these entities intersect in unique ways to facilitate the delivery of Food Is Medicine interventions, contributing to the overall effectiveness and sustainability of these programs.
State Medicaid agencies are instrumental in shaping the framework for Food Is Medicine initiatives through various funding mechanisms and policies integrating food and nutrition services into Medicaid programs.
By managing health care services for Medicaid recipients, managed care organizations can enhance access to nutrition services through incorporation of Food Is Medicine interventions into their care models. Community-based organizations are critical partners in executing Food Is Medicine interventions as the primary providers of food and nutrition services, bringing local knowledge and resources to address specific community needs.
Conclusion
The successful implementation of Food Is Medicine programs relies heavily on the ongoing engagement and collaboration among a diverse array of collaborators. Food Is Medicine interventions require a multisector approach that includes state Medicaid agencies, managed care organizations, health care providers, community-based organizations, and food production partners.
Together, these entities must establish a coordinated framework for member screening, referrals and enrollment, as well as service authorization, delivery, and reimbursement. Additionally, the streamlined utilization of information technology systems is essential for ensuring accurate data tracking, management, and reporting, which are imperative for monitoring program implementation and identifying strengths, challenges, and areas for improvement.
Program evaluation plays a critical role in refining and sustaining nutrition interventions, allowing collaborators to adjust their approaches over time. By assessing the impact on members’ health and well-being, collaborators can advocate for the ongoing integration of Food Is Medicine programs into Medicaid funding streams.
While preliminary research on Food Is Medicine programs has shown promising results, the existing evidence base remains limited due to small sample sizes, nonrandomized comparisons, and variations in intervention length, dosage, and outcome measures. Addressing these limitations through rigorous study designs, standardized measures, and comprehensive evaluations will be essential for advancing the field and establishing the effectiveness of Food Is Medicine interventions.
Recognizing and empowering collaborators as active participants in the design, implementation, and sustainability of Food Is Medicine programs fosters collaborator investment and commitment, which are vital for long-term success. Continued efforts to strengthen partnerships and address implementation challenges will be crucial for the growth and effectiveness of Food Is Medicine initiatives.
Ultimately, a collaborative and adaptive approach will enhance Food Is Medicine programs and promote better health outcomes for the communities they serve.
NOTE: This page contains links to non-United States Government websites. We are providing these links because they contain additional information relevant to the topic(s) discussed in this document or that otherwise may be useful to the reader. We cannot attest to the accuracy of information provided on the cited third-party websites or any other linked third-party site. We are providing these links for reference only; linking to a non-United States Government website does not constitute an endorsement by HHS, or any of our employees. Also, please be aware that the privacy protections generally provided by United States Government websites do not apply to third-party sites.