Food Is Medicine Intervention Components
Food Is Medicine (FIM) interventions are most effective when designed and implemented to align with and build upon the assets of the community context and partners.
The graphic below shows the 4 components to consider for inclusion in all FIM interventions. While contexts differ across settings and geographic regions, we acknowledge these 4 components as essential building blocks of any Food Is Medicine intervention. At the core of any intervention is the provision of food itself — but in an ideal situation, the provision of food is accompanied by navigation and educational supports provided by a care team that could include a range of health professionals with an understanding of the individual’s needs.
As the field continues to evolve, more evidence will become available to inform the design of each component in greater detail.
Types of Food Is Medicine Interventions
Within the unified U.S. Department of Health and Human Services (HHS) Food Is Medicine (FIM), FIM approaches include interventions that have a nexus between the health care system and the community by providing food that can help to manage, treat, and prevent chronic health conditions.
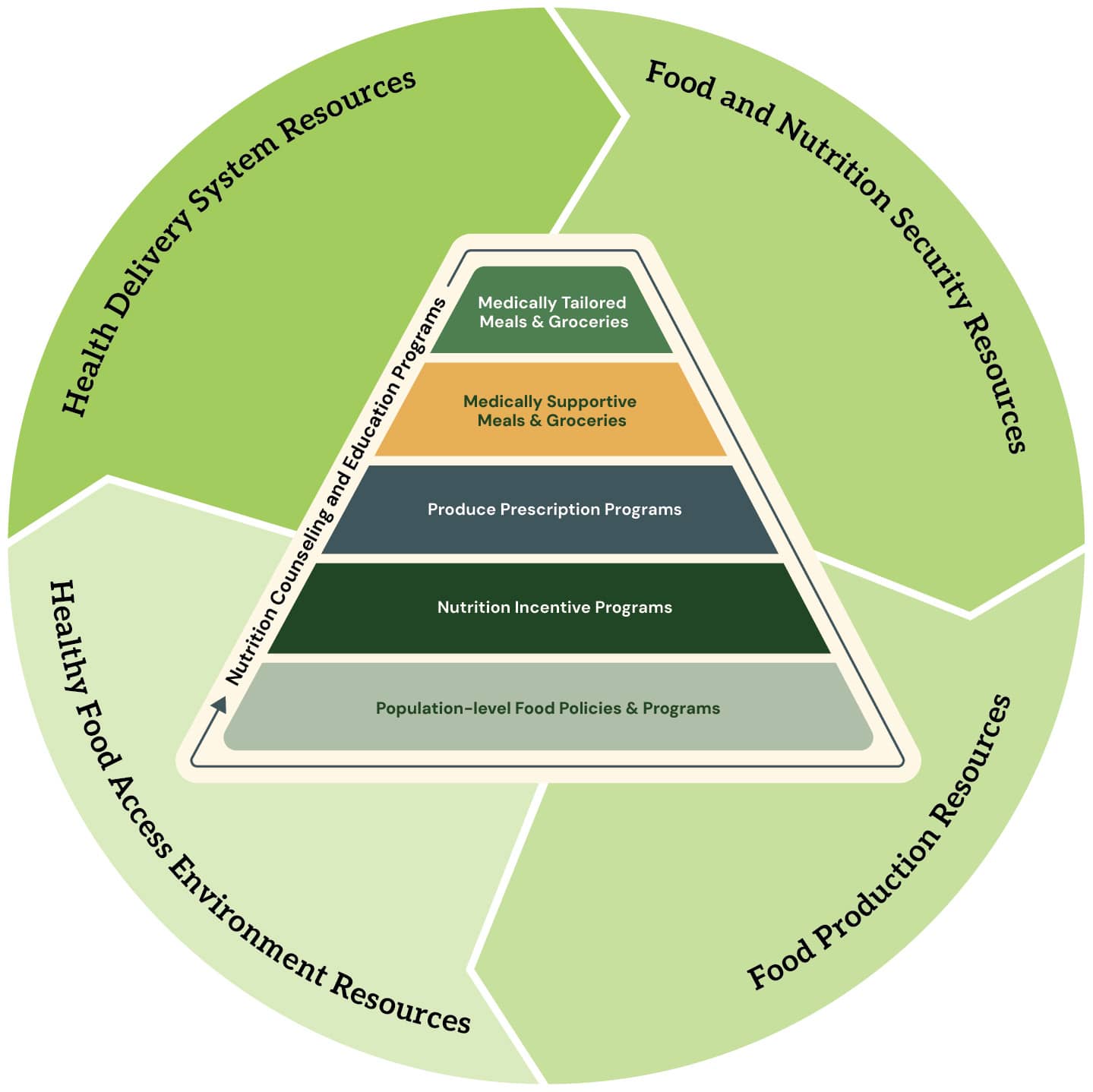
Recent research has conceptualized FIM interventions in a pyramid in which the top tiers (i.e., medically tailored and medically supportive meals and groceries) are typically reserved for patients with the greatest treatment needs, and lower tiers (i.e., produce prescription and nutrition incentive programs) can have much broader impacts for preventive care and reducing the impacts and severity of diet-related chronic illnesses.
The graphic below illustrates our perspective of major FIM interventions, delineating the latest progression of the pyramid framework expressed in the literature. The following sections provide brief descriptions of each intervention.
FIM interventions vary in both what they include — some more comprehensive interventions include food and nutrition counseling or education, and some provide solely food or solely nutrition education — and in how tailored the intervention is in meeting the individual's specific nutrition and health care needs.
Individuals may access FIM interventions through various paths, including within a clinical setting through a referral or prescription from their health care provider or hospital that has identified the need for the intervention.
Alternatively, individuals may access FIM interventions through community access points (e.g., food banks, food pantries, social service providers) and state-based assistance programs or health plan care managers.
Medically Tailored Meals (MTMs)
Medically tailored meals (MTMs) are fully prepared meals that are typically provided to patients with complex medical conditions who are unable to shop and prepare meals on their own. MTMs are provided to patients through a referral from a medical professional or health care plan and are part of a treatment plan for certain diet-related health disease(s) or condition(s).
MTMs are tailored by a Registered Dietitian Nutritionist (RDN) to meet the medical and dietary needs of the patient. Some MTM programs have been shown to improve health outcomes and lower health-related costs. Most MTM programs are designed to serve high-need patients who may participate in the program for longer durations because of their health, age, and other needs. Additionally, most patients would not be able to afford to participate in an MTM program without insurance coverage.
See More Research on MTMs
To explore the potential of MTMs, the National Resource Center on Nutrition and Aging hosted a daylong session where participants heard evidence-based research on health care cost savings from MTM programs and firsthand accounts from 3 programs that employ different models to suit their differing local situations.
- Read the brief summarizing the event and recommendations [PDF - 5 MB] for moving forward.
The Food Is Medicine Coalition (FIMC) wrote a summary of peer-reviewed research studies and white papers conducted by members of FIMC for over a decade to provide a high-level overview of the types of impact that the MTM intervention has had on individuals living with severe, complex, or chronic illnesses. FIMC recently created an Accreditation Program to support consistent, high-quality provision of MTMs.
Medically Tailored Groceries
Medically tailored groceries are perishable and nonperishable grocery items, assembled in a prepackaged box or bag, designed by RDNs to address an individual’s specific needs and health conditions. They generally require additional preparation before consumption.
Patients can access medically tailored groceries through home delivery programs or at distribution sites located in community food pantries or health care settings. Health care providers, health insurance plans, and community-based organizations can screen patients to determine whether they are eligible to receive medically tailored groceries.
Medically Supportive Meals
Medically supportive meals are prepared meals (e.g., heart-healthy or diabetes-friendly meals) provided to an individual to manage chronic diseases or prevent disease in individuals at higher risk for illness. Unlike MTMs, medically supportive meals are generally not tailored to the individual.
While each patient’s treatment plan is unique, medically supportive meals are generally not tailored to accommodate patients’ specific medical and medication histories. Medically supportive meals include healthy foods that can be used by a broad patient population to improve dietary habits and overall health.
Medically Supportive Groceries
Medically supportive groceries include perishable and nonperishable grocery items that are universally healthy and would benefit a broad patient population. Medically supportive groceries are selected by health care professionals for patients with the manual dexterity necessary to cook the groceries before consumption.
Although health care professionals consider each patient’s physical limitations before providing them with medically supportive groceries, they generally do not tailor the groceries to the specific dietary restrictions and chronic diseases of each patient.
Produce Prescriptions (PPRs)
PPRs generally include fresh, frozen, or canned produce with no added salt, sugar, or fat. Individuals with specific nutritional needs and food access challenges can get PPRs from their doctors.
PPR programs enable health care professionals to prescribe a predetermined dollar amount of fruits and vegetables to patients who have experienced or are at risk of experiencing negative health outcomes.
3 types of access points that provide this food at reduced or no cost are private industry (e.g., grocery stores, private grocery delivery services), onsite access points at health care sites (e.g., hospital-based food pantries), and community distributors (e.g., food banks, food pantries). Field experience has shown that a PPR program with a minimum duration of 6 months and ability to re-dose as medically necessary is recommended to improve patient outcomes.
PPR programs may be part of a long-term nutrition and health management plan for patients experiencing chronic diseases. Researchers have recommended that a PPR program’s duration should match each patient’s unique medical needs and allow for re-dosing rather than standardizing program length at a certain number of months.
See Resources on PPRs
Social Determinants of Health: Fruit and Vegetable Incentive Programs
The Community Preventive Services Task Force recommends fruit and vegetable incentive programs for households with lower incomes based on strong evidence of effectiveness in reducing household food insecurity and increasing household fruit and vegetable consumption.
Components of Fruit and Vegetable Programs
The CDC collectively refers to fruit and vegetable voucher incentives and produce prescriptions as fruit and vegetable programs. Those designing or implementing these programs can consider several key components. These include determining community needs, partners, tools and technology, and complementary programs. A community food assessment can help identify assets and gaps in food access to inform program development.
Wholesome Wave Produce Prescription Programs
This report and interactive maps were commissioned by Wholesome Wave to further the evidence-base and policy-change potential for investment in food and health systems through the produce prescription model.
Nutrition Incentive Programs
A nutrition incentive could be a financial or nonfinancial encouragement to purchase healthier foods. Although the goal of nutrition incentives is to improve diet quality and thus control or reduce the risk for chronic disease, recipients typically are not required to have or be at risk of developing a diet-related condition.
Nutrition incentive projects increase the purchase of fruits and vegetables by low-income consumers participating in benefit programs by providing incentives at the point of purchase. Many nutrition incentives build on the foundation provided by certain federal nutrition assistance programs, specifically the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) and the Supplemental Nutrition Assistance Program (SNAP).
Population-Level Healthy Food Programs and Policies
Population level food policies and programs include actions that directly support FIM interventions within community structures to enable greater individual health benefit. Programs and policies are diverse in nature, but they typically address nutrition education or food access. The broad scope of these types of policies and programs facilitate communication and action across sectors.
Examples of programs that could be leveraged to enable FIM include:
- Federal nutrition assistance programs
- Federal nutrition education
- Nutrition labeling and regulatory actions
- Food policy councils
- Healthy food financing initiatives
Nutrition Education and Counseling
Nutrition education and counseling are components of a FIM intervention in many contexts. They help participants to acquire lasting skills and behavioral change.
Nutrition education means:
- Any combination of educational strategies, accompanied by environmental supports, designed to motivate and facilitate voluntary adoption of food choices and other food- and nutrition-related behaviors conductive to health and well-being.
- Nutrition education is delivered through multiple venues and involves activities at the individual, community, and policy levels.
Different approaches to nutrition education and counseling depend on the clinical needs of the patient, but they can range from more intensive Medical Nutrition Therapy (MNT) provided by an RDN to group classes in teaching kitchens to behavioral pharmacy programs. FIM interventions are generally designed to combine direct nutrition education and cooking skills with environmental support of food provision.
Medical Nutrition Therapy (MNT)
MNT is a form of treatment that employs nutrition education and behavioral counseling to prevent or manage a medical condition. The intervention is an evidence-based process that aims to treat or manage a disease through nutrition. Its components are comprehensive and include assessment of nutritional status and provision of nutritional diagnosis, diet modifications, counseling, and specialized nutrition therapies.
RDNs work with patients and other health care team members to identify diet-related health needs, personal goals, and patterns of daily living to ensure the prescribed diet is aligned to and supportive of personal needs.
Culinary Medicine
Culinary medicine takes an evidence-based approach to promoting healthy dietary habits by combining the art of cooking with the science of medicine. Culinary medicine classes both guide practical hands-on food preparation and offer scientific information about how nutrition and dietary patterns affect health.
Medical doctors or RDNs often teach these classes. Outside of the classroom, RDNs also provide nutrition education to help patients manage chronic medical conditions.
Teaching Kitchens
Teaching kitchens can provide instruction in any of the following areas:
- Nutrition education
- Basic cooking skills
- Physical activity and its critical role in health optimization
- Mindfulness and its relationship to diet, portion control, satiety, and resilience
- Web-based resources and technologies to access recipes and nutrition facts
- Motivational interviewing strategies and health coaching techniques to induce sustained behavioral change
Teaching kitchens can be delivered virtually or in person in rural and urban settings. Therefore, besides serving as learning environments, teaching kitchens can provide a space for nutritious food distribution programs to be accessible to diverse populations.
Teaching Kitchen Collaborative Impact
Read the 2023 Impact Report from the Teaching Kitchen Collaborative to learn more about the usefulness of hands-on and virtual teaching kitchen programs.
Behavioral Pharmacies
Behavioral pharmacies are educational delivery systems for behavioral prescriptions that offer:
- Access to physical activity
- Healthy food provision
- Social support
- Stress reduction to improve patient care
The primary goal of behavioral pharmacies is to connect patients to a healthy, thriving community. After being prescribed a behavioral prescription by their health care provider, patients participate in in-person meetings and receive support from their peers and coaches to achieve the health goals set by their doctors.
Behavioral pharmacies strive to embed behavioral factors that improve health into the health care system by making them readily accessible and affordable. Behavioral pharmacies can be coupled with other educational approaches to optimize sustainable dietary habits.