Payer Participation
Shows the impact that private insurance providers can have on advancing Food Is Medicine (FIM) initiatives, improving overall patient health, and lowering medical costs.
Targeted Programs
Assesses unmet health related social needs of its members to inform local implementation of its health care and FIM interventions.
Value-based Care
Develops a value-based care model that incentivizes providers to address SDOH and prioritize whole-person health through integrated social and clinical care.
Bright Spot Profile
Highmark, based in Pittsburgh, PA, serves approximately seven million members in geographically and ethnically diverse communities across Pennsylvania, Delaware, New York, and West Virginia. Highmark takes a whole-person approach to clinical and social care; thus, Highmark integrates its FIM efforts across its enterprise.
Highmark’s FIM programs provide healthy food, nutrition education, and social care to populations that are underserved in a manner that aims to account for and overcome social barriers to care.
Highmark was included in the Bright Spot series to show how the participation of private payers in advancing FIM initiatives can greatly improve patient health outcomes and lower health care costs, especially when payers integrate FIM initiatives into existing infrastructure and services while keeping social barriers to care in mind.
Highmark FIM Efforts
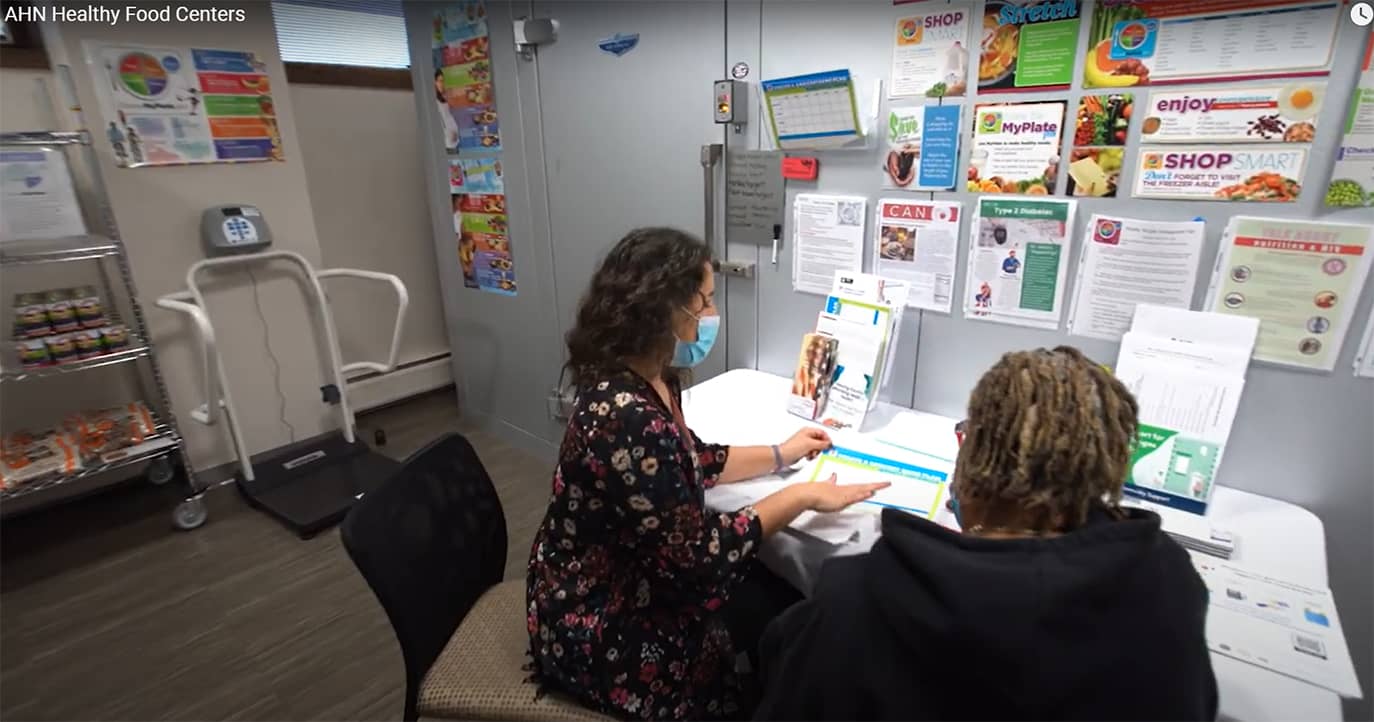
Implementing Healthy Food Centers in Hospitals
Highmark launched its first FIM program, the Allegheny Health Network (AHN) Healthy Food Centers (HFCs), in 2018. HFCs provide patients access to healthy food — in some cases from community gardens — as well as nutrition counseling to improve patients’ overall health. Because they are based in hospitals, HFCs enable providers to prescribe food in conjunction with medical care for patients who screen positive for food insecurity. The centers are also accessible to patients with transportation barriers, as their locations are accessible via public transit. Furthermore, HFCs have no income threshold, expanding access to healthy food for more people.
As of the time of publication, the HFCs have served over 49,000 people equating to approximately 490,000 meals.
Across all sites, all-time data indicates the following:
- Of patients beginning in the severe range (> 6 mg/dL), Hemoglobin A1c averages went from 11.1 pre-HFC to 8.7 after 6 months
- Of patients in high blood pressure (hypertension) stage 2, average systolic blood pressure went from 150.8 pre-HCF to 137.2 after 6 months, and average diastolic blood pressure went from 89 to 82.3
- Of patients in the severe cholesterol range (overt 240 mg/dL), averages went from 277.6 pre-HFC to 223.5 after 6 months
- Of patients in the severe HDL (high-density lipoprotein) cholesterol range (less than 40 mg/dL) averages went from 32.3 pre-HFC to 36.7 after 6 months
Establishing the West Virginia Healthy Neighborhood and Food for Mountaineers Programs
The Highmark West Virginia Charitable Fund for Health and the Highmark Foundation collaborated to launch the West Virginia Healthy Neighborhood and Food for Mountaineers programs in 2023 and 2024, respectively, to serve critical food and nutritional needs of its members in West Virginia.
West Virginians face high rates of food insecurity, obesity, and diabetes, demonstrating the intersection of food security and diet-related chronic diseases. Both programs aim to address this challenge by increasing participant access to nutritious food through grants that fund restricted-use debit cards to purchase nutritious food at Dollar General, Food Lion, Kroger, and Walmart stores. The total grants are worth $2.5 million over 3 years and have so far reached over 600 individuals and over 1,400 household members.
These programs demonstrate that addressing core needs like food often helps individuals engage more deeply in their health, impacting a wide range of outcomes and the long-term cost of care. This collaboration between health care payers and providers is also critical muscle memory for the long-term work of moving toward more value-based care.
Marginalized Groups
Highmark aims to make its FIM programs as inclusive as possible by establishing relationships with communities that are traditionally marginalized. Those communities include:
- Low-income zip codes
- Rural and economically disadvantaged former coal fields
- Predominantly Black census tracts
- Predominantly Hispanic census tracks
Highmark aims to best serve communities that are marginalized by tailoring its programs to the needs of individuals in those communities.
Whole-person Approach
Tailor Programs to Address Unmet Needs
Highmark acknowledges that health is largely influenced by SDOH. To address this challenge, Highmark collaborated with partners across their integrated delivery network to develop and implement a universal SDOH assessment that can be administered in-person, digitally, and telephonically.
By integrating the assessment and community support referral platform into their case management model and systems, clinicians are able to identify barriers for individual members and patients and quickly connect them to resources. As of July 2024, Highmark Health has conducted over 1.7 million assessments to identify social barriers of health. This data also helps inform investments in population- and condition-specific SDOH interventions.
Strengthen Collaboration Between the Health Sector and CBOs
In 2022, Highmark launched the High-Performing Social Care Network (HPSCN) in western Pennsylvania to foster collaborative efforts between the health care system and community-based organizations (CBOs).
The HPSCN financially incentivizes CBOs to address social needs, such as food insecurity, housing instability, social isolation, and lack of adequate transportation, for patients referred by the health sector. It streamlines communication between clinical staff and CBOs through the Community Support Platform powered by findhelp, a website that connects individuals to free or reduced cost resources. The model enables clinicians to connect patients to social care to address SDOH that negatively impact patient health, ultimately reducing health expenditures in the long-term.
HPSCN experienced early success and positive reception. Initially, the network consisted of 20 CBOs, but as of 2023, the network expanded to include 37 CBOs across multiple counties in Pennsylvania. As of July 2024, nearly 900 individuals received help from CBO partners through the network, and the program reported the following positive outcomes based on participant surveys:
- 98 percent of participating CBOs noted that they would recommend the HSPCN to other CBOs
- 90 percent of participating CBOs felt that the HSPCN enhanced communication between their organization and the health care sector
- 93 percent of clinical teams surveyed felt that the HSPCN added value to their teams
Fostering Partnerships
Highmark attributes the success of its FIM and value-based programs to its efforts in fostering both internal and external partnerships. For example, when creating the Universal SDOH Assessment Tool, Highmark needed to coordinate consensus from more than 9 departments and institutes with different workflows and regulatory oversight.
Community members and CBOs also play a major role in designing and executing Highmark’s FIM programs. Community members provide lived experience to help inform strategy and focus areas, while CBOs are crucial for local-level implementation of FIM programs. To foster its productive partnerships, Highmark devotes considerable time and resources to cultivating and onboarding non-profits and sharing bi-directional feedback to improve program operations and better align incentives to desired outcomes.
The power of CBO engagement is demonstrated with the HSPCN, which requires dedicated involvement from many partners across sectors. Highmark views collaborative efforts like HSPCN as living proof that similar pilot programs can work through 1115 Medicaid demonstrations and statewide navigation systems across the country.
Guidance for Implementers
Pursue Value-based Contracts
Overburdened clinicians are one major challenge Highmark continues to face when implementing its FIM interventions. As a result, any additional processes and interventions that rely on provider networks need considerable buy-in and financial incentives. One way to overcome this challenge is through value-based contracts, which arrange payment for health care services to be tied to patient health outcomes rather than the services provided alone.
Many successful Highmark programs, such as HSPCN, the West Virginia Healthy Neighborhood program, and the Food for Mountaineers program already operate under, or are moving toward, value-based arrangements.
Report the Cost of Interventions
Many published studies on the impact of FIM services do not include real data on the cost of interventions. This misalignment between existing research and the cost of implementation will limit widespread, sustainable adoption of FIM interventions.
Adapt Processes for CBOs
The level of compliance and complexity required by health plans can complicate working with CBOs, but health care systems can adapt their procurement, business processes, and language to better collaborate with community groups. Some community groups, however, might need to build new data and business process capabilities.
Adopt a whole-person approach
Highmark programs demonstrate the power of taking a whole-person approach to FIM and health care. For example, preliminary analysis indicates that the impact of both the HFC and HPSCN seems to be largest with individuals who receive both social and clinical care. This finding supports the hypothesis that an integrated, whole-person approach will produce the greatest results, particularly for individuals with limited prior engagement with the health care system.
Next Steps
- Highmark plans to expand the HSPCN model.
- Highmark included the HSPCN in its successful application to serve as a managed care organization for the West Virginia Medicaid Population. Highmark plans to launch a similar social care network in West Virginia in Fall 2024.
- First Steps and Beyond — a community collaborative to reduce black infant and maternal death in Allegheny County spearheaded by Allegheny Health Network — recently received a grant from the American Heart Association to provide food cards and nutrition education to birthing people participating the program.